Manuscript
Introduction
The finding of a chorionic bump on ultrasound in the first trimester of pregnancy was initially described by Harris et al as a convex protuberance, with an irregular surface, located on the choriodecidual surface and protruding inward of the gestational sac(1). The reported incidence of chorionic bump ranges from 1.5 to 7 per 1000 pregnancies and is often found incidentally(2). It is a low frequency condition and is not familiar among people who perform obstetric ultrasound examinations. The presence of a chorionic bump is considered a risk factor for a non-viable pregnancy; if it is only an isolated finding, most end up in a live newborn.(3) There is evidence that suggests a guarded prognosis when chorionic protuberance is present, even the risk of spontaneous abortion could be doubled when found on ultrasound in the first trimester(2). We report the case of a primiparous woman and the sonographic findings related to the presence of a chorionic protuberance in the first trimester.
Clinical case
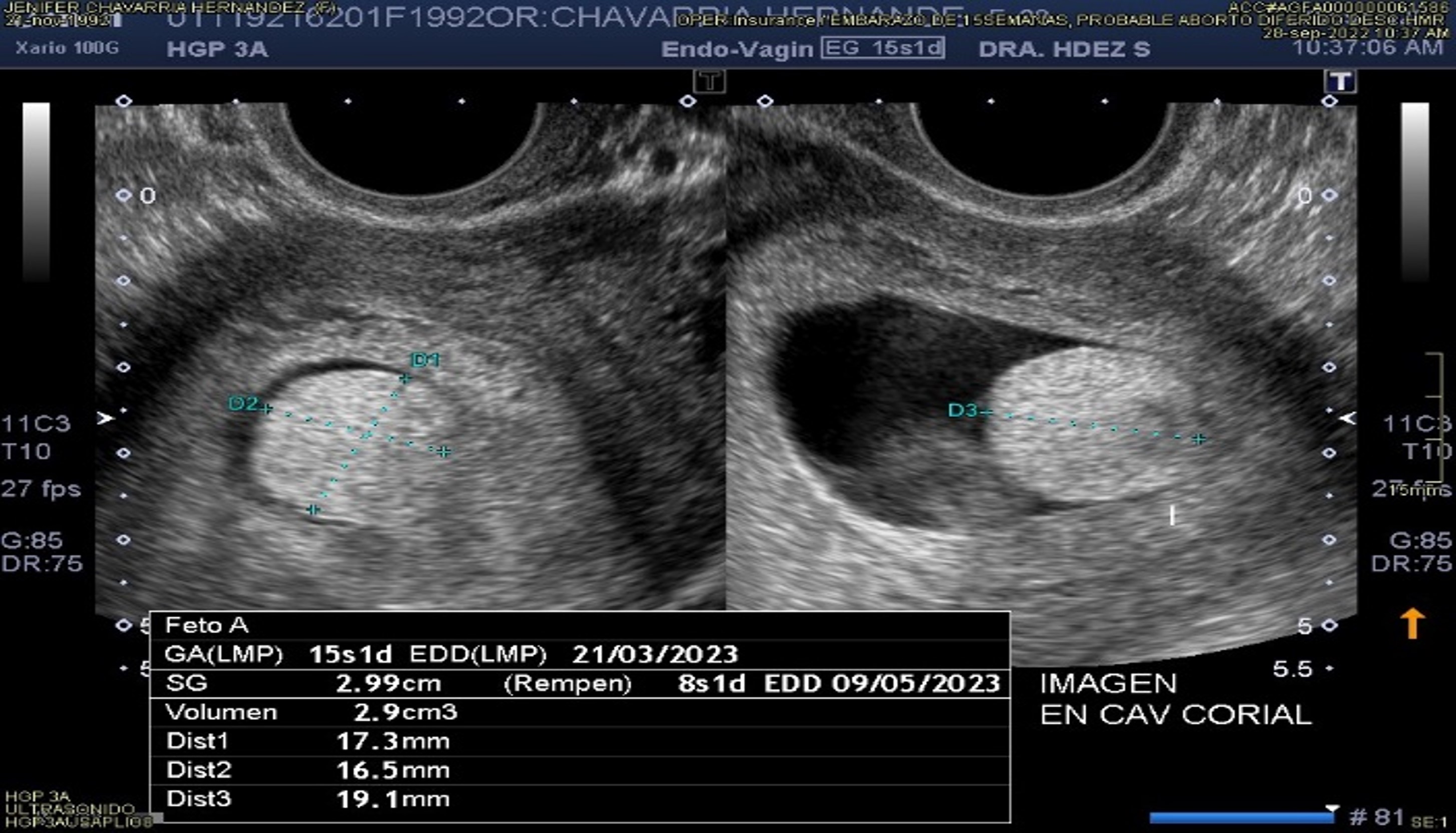
This is a 29-year-old patient who came for a medical check-up because she reported a delayed menstrual period and a positive urine pregnancy test, in addition to her own pregnancy symptoms. Information is collected from the patient, finding in the anamnesis hereditary family and personal pathological antecedents of no importance to the current condition. In the gynecologic and obstetric history, she has a history of menarche at 10 years of age, with irregular menstrual cycles, and she has interrupted intercourse as a method of family planning. At his visit, he presented only with symptoms of nausea and a history of vomiting of gastric contents on 2 occasions in the previous 24 hours, without referring to transvaginal bleeding. On physical examination, no significant findings were found, the cervix was closed and long, with no transvaginal leaks or discharges. We proceeded to corroborate the diagnosis with an immunological test in pregnancy blood, reporting positive, for which it was decided to perform a vaginal ultrasound. This ultrasound examination concluded: Uterine cavity with an irregular gestational sac with a mean diameter of 29.9mm with poor decidual reaction, observing amnion inside without evidence of an embryonic pole, with a 2.3mm yolk sac. In the chorionic cavity, a hyperechogenic ovoid image is observed, without vascular flow, measuring approximately 17.3 x 16.5 x 19.1mm. Cylindrical cervix without apparent lesions, 43.8mm long, both laterouterine ovaries with anechoic images suggestive of follicles. No image suggestive of free fluid in the posterior fornix. The ultrasonographic study established the Diagnosis: 8 weeks gestation due to gestational sac, anembryonic pregnancy, chorionic protuberance, ovaries with follicles (Figure 1 and Figure 2). For these reasons, definitive surgical treatment with dilation and curettage was decided, sending the tissue collected from the curettage procedure for complementary histopathological study. It was expected that the results would show sections or cystic-based areas in the histopathological study with the possibility of finding fibrin tissue and/or scattered chorionic villi covered by cytotrophoblasts and syncytiotrophoblasts, as has been seen in other publications (10). However, in our histopathological analysis report, it showed: abundant ovulodecidual remains, various fragments of irregular tissue which together measure 7x4.5x2cm, with areas of a light brown membranous appearance, alternating areas of a hairy, light and dark brown appearance, the tissue presents data of non-specific moderate acute deciduitis with focal microabscess in addition to first trimester chorionic villi and Arias-Stella reaction.

Figure 1. Gestational sac with chorionic bump, in addition to embryo (without cardiac activity) and yolk sac.
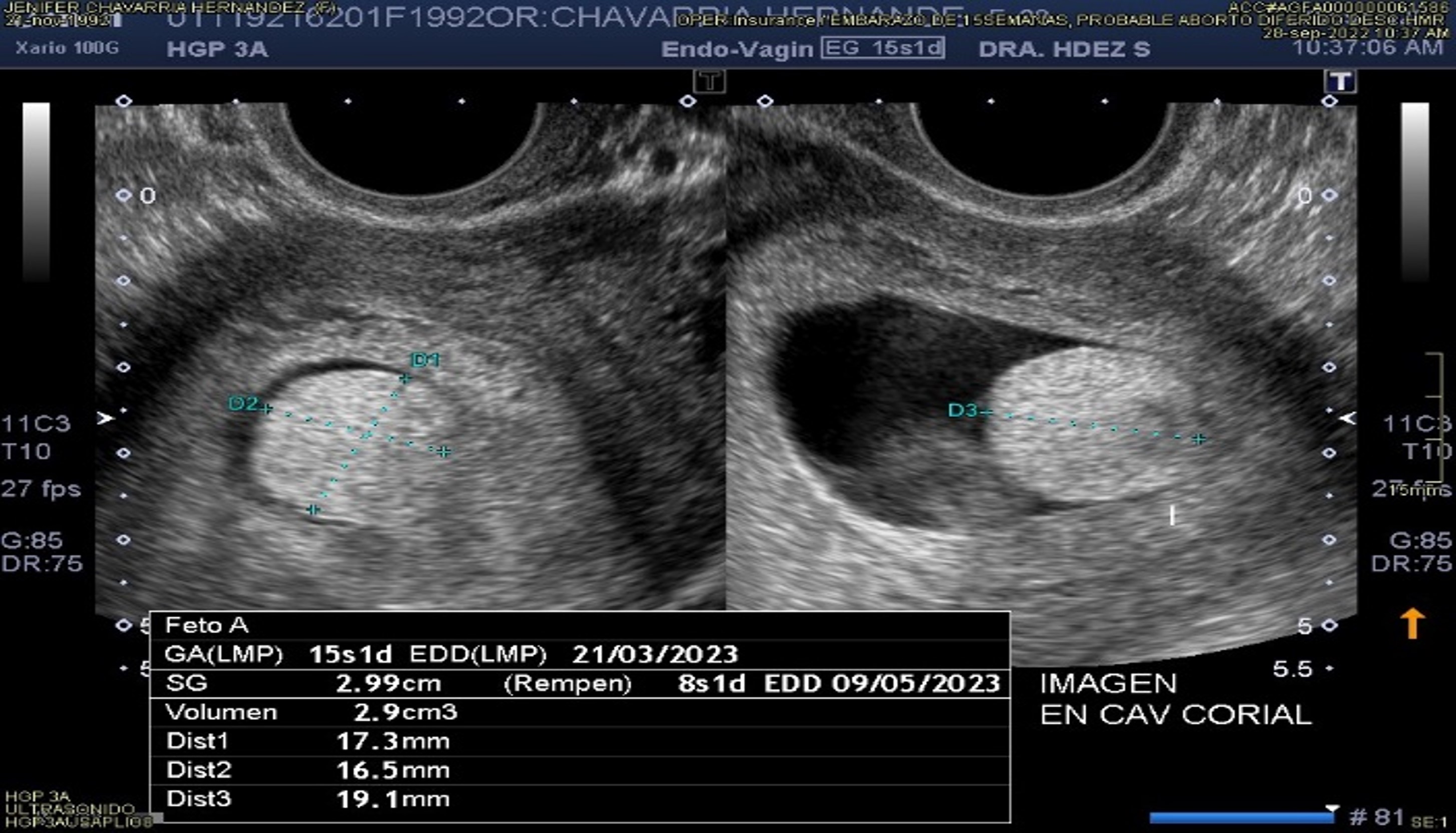
Figure 2. Gestational sac that has a chorionic bump inside.
The patient after her surgical event had no complications, so she went to the recovery service and progressed favorably, so she was discharged 24 hours after the immediate post-surgery with prophylactic antibiotic treatment.
Discussion
The case that we present provides additional evidence on the ultrasonographic finding known as chorionic protuberance. First, we present information on the case and on its ultrasound appearance in the first trimester of pregnancy. To date, most reports have described spontaneous resolution of the chorionic pons in the vast majority of reports. Our case, however, demonstrates that, on some occasions, a Chorionic Protuberance may be present and associated as a Finding of poor obstetric evolutionary prognosis. In this sense, ultrasound is a tool capable of assessing the presence and size of the Chorionic Protuberance, especially if it is detected in a very early pregnancy(4). Some authors suggest that if normal fetal growth is confirmed in follow-up scans, the risk of pregnancy loss is greatly reduced(5). In fact, once the pregnancy reaches the end of the first trimester, the pregnancy prognosis in such cases is generally good(5).
Continuing with our case, we describe an unusually poor prognosis early prenatal course associated with an ultrasonographic finding (chorionic protrusion) in the first trimester. This last condition that is described as an image in chorionic cavity hyperechogenic ovoid, without vascular flow that protrudes from the embryonic surface surrounded by a thin membrane and contains areas of echogenic material. There are different authors who believe that this fact is the result of bleeding from the area close to the umbilical cord or the insertion site, secondary to traction and rupture of the fetal vessels that run below the amniotic membrane(6).
In these cases, transvaginal bleeding is not present as in our case, since the amnion firmly contains the clot. Thrombus retraction may produce, over time, the characteristic sonographic features of a subamniotic hematoma with echogenic material retracting at its base surrounded by the layer of the anechoic portion. Therefore, it is suggested that there could have been another pathophysiological mechanism for a subamniotic hematoma, which could have favored the fatal outcome of the embryo in our study. It is for this reason that said hematoma remains covered by the amnion and that it usually does not grow during the rest of the pregnancy. However, adequate surveillance should be carried out in this type of case, since some authors have postulated that large subamniotic hematomas may be associated with fetal growth restriction and/or early embryonic death(6). An additional associated risk is related to its location; if they are close to the umbilical cord insertion site, and especially if they are large, they can compress the placental vessels and the umbilical cord, leading to adverse fetal outcome(10).
A potential limitation of our study was the fact that the precise umbilical cord insertion site was not determined in the first trimester and the subamniotic hematoma could have developed earlier without being related to the presence of chorionic protrusion, which could be the cause of the umbilical cord. embryonic death. However, at the time the chorionic bump was detected, there were no other findings on the surface of the placenta to suggest coexisting conditions. As stated above, there are few studies in which only one report of a Chorionic Protuberance progressing to a subamniotic hematoma has been previously described(7, 8).
There have been reported cases in which patients, upon discovering a chorionic protuberance, underwent aneuploidy detection studies of fetal DNA in maternal blood during the first trimester. These studies yielded positive results for trisomies, which were further supported by obtaining a chorionic villus biopsy. The diagnosis was subsequently confirmed through chorionic villus sampling at 12 weeks of gestation. In these instances, the patients opted to terminate the pregnancy. As a result, histopathological analysis of the extracted tissue was conducted, revealing characteristics of immature villi tissue along with hydropic villi and decidual edema.(8).
Wax et al. propose that a sonographically isolated chorionic bump could substantially elevate the chances of fetal chromosomal abnormalities in pregnancies with heightened aneuploidy risk. This holds significance for patient counseling. Despite the hematoma hypothesis and the identification of coagulation problems in certain patients, there was no notable link between coagulopathy and successful live births among individuals with a chorionic bump.
However, the documentation available in this case suggests that the chorionic bump may have resulted from a subamniotic hematoma, which may have been the cause of the poor embryonic prognosis. Finally, different authors agree with the fact that chorionic protuberance could be considered a risk factor for non-viability in pregnancy(9). Likewise, if it is detected in the first trimester, it is ideal to monitor and follow-up by ultrasound, even to look for it in ultrasound scans in the second or third trimester.(10).
Conclusion
"Chorionic bump" remains a little-researched phenomenon in early pregnancy ultrasound. The etiology is still unknown, but it would represent a small hematoma. Although it is diagnosed infrequently, when first identified, it can be associated as a finding of poor prognosis. The most important task for the sonographer is to know how to correctly identify it and differentiate it from early embryonic death. Other studies need to complement the characteristics found so far in this infrequent ultrasound finding.