Manuscript
Introduction
Gestational surrogacy (GS), also known as uterine surrogacy, is a well-known assisted human reproduction technique recognized by the World Health Organization (WHO). The process involves an individual or couple known as intended parents (IP) who receives assistance from a woman who lends her uterus to carry out the pregnancy (gestational carrier (GC)). This type of treatment is presented as an option for individuals who, for various medical, sexual, or gender reasons, are unable to fulfill their procreational desires. There are two main types of surrogacy: traditional and gestational. In traditional surrogacy, the surrogate mother's oocytes are used, making her a genetic parent along with the intended father. Gestational surrogacy, on the other hand, involves transferring an embryo from the intended parents or from donated gametes to the surrogate's uterus. In gestational surrogacy, the GC has no genetic connection to the child [1].
The first gestational surrogacy treatments date back to the late 1980s in the United States, and the first GC was identified as such in 1985 [2]. Since then, there has been a significant grow in the practice of gestational surrogacy in that country, with an increase of over 470% [3]. Worldwide, the demand for gestational surrogacy has been steadily expanding due to various reasons, including the complexity of adoption processes. According to a 2017 report from Cornell Law School (USA), only 14 countries worldwide allow gestational surrogacy. The report also notes that in 21 countries this practice takes place without economic compensation, and in 39 there is no regulation related to economic aspects. Regarding the prohibition of gestational surrogacy, the study mentions 50 countries that prohibit it and 72 that have not made any official stance on the matter [4].
According to the International Federation of Fertility Societies (IFFS) Surveillance 2016, doctors from 65 countries responded the following to the question, "Is gestational carrier arrangements permitted in your country?": Respondents from 24 countries (38%) noted that gestational carrier arrangements are allowed by statute or guidelines, respondents from 36 countries (56%) reported that it was not allowed, respondents from 8 countries were not able to answer the question and respondents from 8 countries that allow gestational carrier arrangements noted that traditional gestational carrier arrangements were not allowed [5].
In Argentina, there is currently no law regulating gestational surrogacy practices. According to Article 19 of the Argentine National Constitution, what is not prohibited is allowed, and this is the main reason why the first treatment was performed by Halitus. This legal loophole has led many patients to elevate claims to the corresponding legislative authorities in an attempt to draw attention to this deficit. Despite this lack of regulation, the scientific team at Halitus Instituto Medico in Buenos Aires began, over a decade ago, the creation of interdisciplinary teams to provide appropriate coverage and scope for this demand. We believe that care and follow-up should be equal for all parties involved, being able to support each one based on their individual needs. In this regard, the coordination of medical intervention with proper legal advice and ongoing psychological intervention throughout the process allowed for the first successful birth through gestational surrogacy in Argentina in 2011. Subsequently, legal precedent was established in 2013, marked by a magistrate's approval of the registration of the child born through this method directly under the names of her procreational parents [6].
The journey was long until 2017 when, thanks to a collective action by several LGBTQ+ families, a law was passed allowing babies born via GS in the city of Buenos Aires to be registered under the name of the procreational parents, provided that the following conditions are met before the treatment is performed: 1) they are minors born in the Autonomous City of Buenos Aires through the method of collaborative gestation; 2) the procreational intent of the parents has been expressed beforehand, freely, and informed; 3) the GC has unequivocally expressed a lack of procreational intent, and 4) the registration must be done preventively, with the GC data recorded in the file [7]. Currently, the registration process for newborns through gestational surrogacy in the Autonomous City of Buenos Aires is regulated by Directive 122/2020 of the “Dirección General del Registro del Estado Civil y Capacidad de las Personas” [8].
To ensure proper guidance and care for all parties involved, it is essential that a multidisciplinary team evaluate both the IP and the GC. This involves medical and psychological assessments, as well as legal advice, to carry out the treatment appropriately and safely. The creation of interdisciplinary teams for this purpose requires professionals not only proficient in their respective fields but also trained in this specific area. The presence of specialists in law, medicine, and psychology allows for the creation of recommendations to advance and sustain this practice in the absence of a regulatory legal framework. While gestational surrogacy in Argentina lacks a specific law, it is governed by multiple professional regulations that make it a feasible and secure practice.
The main objective of this study was to evaluate and share the experience of our Surrogacy program at Halitus Instituto Medico, which is the first one of its kind in Argentina. The study aimed to identify and describe demographic, physiological, social, and treatment-related factors associated with successful surrogacy outcomes.
Materials and Methods
This is a retrospective cohort study to assess the 12-year experience of a Surrogacy Program at Halitus Instituto Médico.
Data collection and extraction
A retrospective identification of all clinic consults for surrogacy was performed. Anonymized data on 1152 surrogacy consults occurring between 2011 and 2023 was extracted directly from the clinic database. Data abstractor had experience in the field of uterine subrogation. All protected health information (PHI) was excluded from the data extraction. Inclusion criteria: All consults for uterine subrogation at Halitus Instituto Médico occurring between 2011 y 2023. Exclusion criteria: Cases with any missing data on main variables as described above. Determination of main variables to be extracted and definition of categories for each variable was determined by a panel of experts on the field. Main variables extracted included: age of intended parents, sex and gender, type of partner, diagnosis, type of treatment and pregnancy outcome.
The intended parents are responsible for the recruitment of surrogate mothers. The clinic is not involved in this process but is responsible for the medical and psychological evaluation and legal advice. All surrogate mothers must be of legal age (+18 years old), and preferably between the ages of 21 and 45 years. Certain situations may dictate the use of a carrier older than 45 years, but all parties involved must be informed about the potential risks of pregnancy with advancing maternal age. The carrier should have had at least one, term, uncomplicated pregnancy before being considered as a GC for the IP. She should not have had more than a total of 5 previous deliveries and no more than 3 deliveries via cesarean section and must have a stable family environment with adequate support to help her cope with the added stress of pregnancy [9]. They should not have any contraindications for pregnancy and should have a low obstetric risk.
During the psychological assessment of potential surrogate candidates, their motivations and treatment expectations are carefully evaluated. Family and group support are provided, if necessary, especially in addressing the repercussions of their decision. Fantasies, fears, and concerns are clarified, evaluating the resources and attitudes of each gestational carrier (GC). The detection of any ongoing psychological disorders is crucial. The previous maternal experience during pregnancy, childbirth, and the postpartum period is also considered.
Independent legal advice is mandatory for both procreational parents and gestational carriers. The legal team is experienced on how to register newborns in Argentina, and about the laws of the country where the parents and the baby will reside if they are foreigners. This point is crucial, as each country has very different legislation regarding children born in other countries whose parents decide to return to their country of origin.
The surrogate mother's endometrial preparation involves oral administration of valerato de estradiol 4 mg twice a day (Ronfase®) until achieving a minimum endometrial thickness of 7 mm and maintaining blood progesterone levels less than 1 ng/ml. Once these conditions are met, vaginal micronized progesterone is initiated at a dose of 400 mg twice a day (Utrogestán®). Since 2021, blood progesterone levels are measured the day before embryo thaw. If the progesterone levels fall between 7 and 10 ng/mL, subcutaneous progesterone at a dose of 25 mg/day (Aleterpure®) is added to the endometrial preparation. If levels are below 7 ng/mL, the embryo thaw is canceled and rescheduled. Embryo transfer takes place after 5 complete days or 132 hours after the start of progesterone.
The formation of embryos was carried out using either the intended parents' own gametes or donated gametes. For ovarian stimulation of the intended mother, antagonist protocols were utilized, along with recombinant follicle-stimulating hormone (rec-FSH) and either urinary-derived menopausal gonadotropin (UP-hMG) or recombinant luteinizing hormone (rec-LH) based on ovarian stimulation protocols. Final oocyte maturation was induced with either recombinant human chorionic gonadotropin (rec-hCG) or GnRH analogs, depending on the ovarian follicle count on the day of trigger. All fertilizations were performed using intracytoplasmic sperm injection (ICSI). Most cycles involved cryopreservation for future embryo thaw transfer cycles, but in some cases, fresh embryo transfers were performed. This segmentation of cycles was done for synchronizing the gestational carrier or for cases involving preimplantation genetic testing for aneuploidy (PGT-A). In the case of a fresh embryo transfer, the cycle synchronization between the intended mother and GC was achieved using contraceptive pills.
Some patients brought their embryos previously cryopreserved in other centers (either in Argentina or other countries), to Halitus. All patients were offered genetic studies for preimplantation genetic testing for aneuploidy (PGTA) and panels for monogenic diseases, but not all chose to undergo these tests. Not all transferred embryos underwent PGTA test.
The study was approved by Halitus ethics committee and waiver of consent was granted by the ethics committee as all data included in the analysis was anonymized.
Statistical Analysis
A convenience sampling method was used. All participants with missing data were excluded from the analysis. Categorical variables are expressed as frequencies and percentage of occurrence. Continuous variables are expressed as means [95% confidence intervals (CI)] or median [interquartile range (IQR)] depending on distribution. Independent samples t-test or Mann-Whitney test were used to assess continuous variables based on the data’s distribution, while categorical variables were compared using the chi-squared test or Fisher’s exact test, where appropriate. Logistic regression models, Odds Ratios (95%CI) and Fisher exact test were computed to identify associations of different factors to successful surrogacy outcomes. All statistical analyses were performed using SAS 9.4 software (SAS Institute Inc., Cary, NC USA), with the risk of Type I error set at α=0.05.
Results
Over a period of 12.5 years (from April 2011 to September 2023), 1152 consultations were held by individuals expressing the desire for uterine surrogacy. Among these, 161 patients (14%) decided to proceed with the treatment. The average age of the patients who consulted was 41.7 years, with the oldest being 70 years and the youngest 18 years old.
The rise in consultations throughout the years is remarkable, even in the face of a global pandemic (Figure 1).

Figure 1. Number of consults per year from 2011 until 2023.
Among the interested patients, 745 (64.67%) were heterosexual couples, 225 (19.53%) were same-sex couples, and 182 (15.8%) were single-parent projects, of which 121 (10.5%) were men and 61 (5.3%) were women (Table 1).
|
OWN-N |
| Age |
41.69 (41.28-42.10) |
| Type of Couple |
|
| Heterosexual couples |
739 (64) |
| Same-sex Male couples |
225 (20) |
| Single Male |
127 (11) |
| Single Female |
61 (5) |
| Diagnosis |
|
| Male Patients |
346 (30) |
| Obstetric Factor |
293 (25) |
| Uterine Factor |
254 (22) |
| Recurrent Implantation Failure |
110 (10) |
| Without clear indication |
71 (6) |
| Advanced Age |
70 (6) |
| Endometriosis |
7 (0.9) |
| Trans Female |
1 (0.1) |
| Completed Procedure |
|
| NO |
991 (86) |
| YES |
161 (14) |
* Data presented as mean (95% CI) or n (%).
Table 1. Characteristics of all consults between 2011 and 2023.
The reasons for consultations from patients interested in this practice were: male patients 346 (30.4%), obstetric factors 293 (30.4%), uterine factors 254 (22.05%), recurrent implantation failure 110 (9.55%), unclear indication 71 (6.16%), advanced age 70 (6.08%), endometriosis 7 (0.61%), and transgender female 1 (0.09%) (Table 1). More detailed diagnoses are shown in Table 2.
|
N |
% |
| Male Patients |
|
|
| Same sex couple |
225 |
65.02 |
| Single Male |
121 |
34.98 |
| Obstetric Factor |
|
|
| Pregnancy contraindication |
202 |
68.94 |
| Recurrent Abortion |
65 |
22.18 |
| ICC |
18 |
6.14 |
| Thrombophilia |
8 |
2.73 |
| Uterine Factor |
|
|
| Hysterectomy |
182 |
71.75 |
| Utierine malformation |
30 |
11.81 |
| Miomatosis |
19 |
7.48 |
| Uterine synechiae |
10 |
3.93 |
| Endometrial cancer |
5 |
1.96 |
| Cervical cancer |
4 |
1.57 |
| Thin endometrium |
3 |
1.18 |
| Arteriovenous malformation |
1 |
0.39 |
| No indication |
|
|
| No desire to get pregnant |
65 |
91.54 |
| Fear of pregnancy |
6 |
8.45 |
Table 2. Detailed Diagnoses of the initial consults.
Finally, 161 cases of uterine surrogacy were carried out. 51% of the treatments were performed by heterosexual couples, 30% by male same-sex couples, 13% by single men, and 6% by single women (Table 3). The average age of the procreational parents was 40.26 years. The diagnostic indications for uterine surrogacy are shown in Table 3.
|
All Participants (n=161) |
+Pregnancy (n=127) |
-Pregnancy (n=34) |
| Age |
40. 26 (39.32-41.20) |
40.03 (38.95-41.12) |
41.12 (39.06-43.17) |
| Type of Couple |
|
|
|
| Heterosexual couples |
82 (51) |
59 (46) |
23 (68) |
| Same-sex Male couple |
48 (30) |
43 (34) |
5 (14) |
| Single Male |
21 (13) |
18 (14) |
3 (9) |
| Single Female |
10 (6) |
7 (6) |
3 (9) |
| Diagnosis |
|
|
|
| Male Patients |
67 (42) |
59 (46) |
8 (24) |
| Obstetric Factor |
37 (23) |
29 (23) |
8 (24) |
| Uterine Factor |
33 (20) |
22 (17) |
11 (32) |
| Recurrent Implantation Failure |
16 (10) |
9 (7) |
7 (21) |
| Advanced Age |
7 (4) |
7 (6) |
0 (0) |
| Endometriosis |
1 (1) |
1 (1) |
0 (0) |
| Oocyte source |
|
|
|
| OD |
133 (83) |
111 (87) |
22 (65) |
| Own |
28 (17) |
16 (13) |
12 (35) |
| Type of Treatment/Embrio Transfer (ET) |
|
|
|
| Crio OD |
97 (60) |
79 (62) |
18 (53) |
| Fresh OD |
36 (22) |
32 (25) |
4 (12) |
| Crio OWN |
20 (12) |
11 (9) |
9 (26) |
| Fresh OWN |
8 (5) |
5 (4) |
3 (9) |
Table 3. Characteristics of the population that completed treatment.
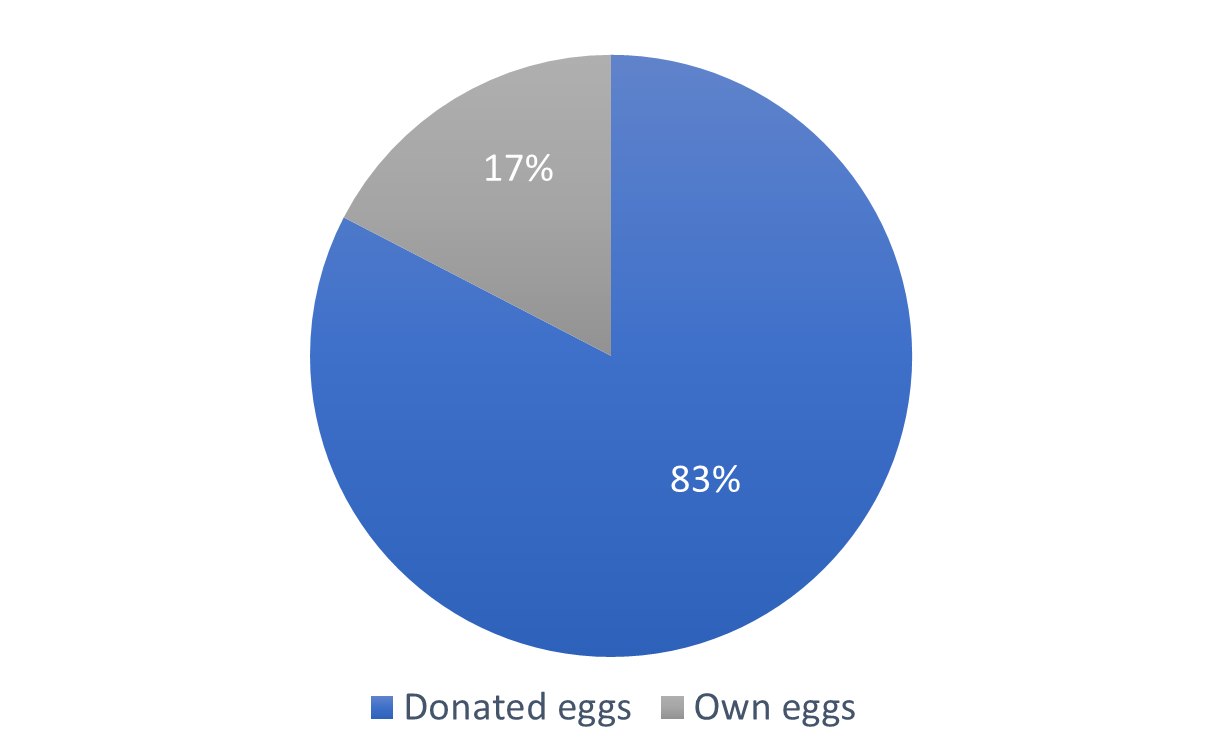
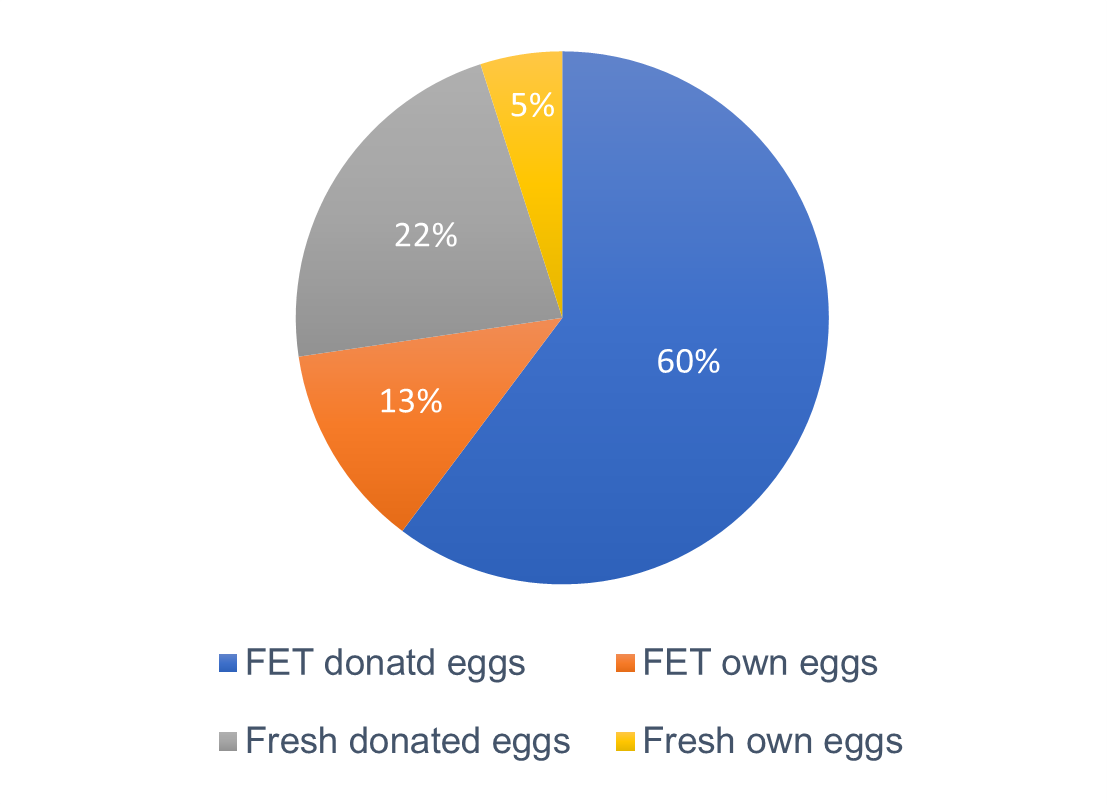
There were 133 treatments with oocyte donation and 28 with own eggs (Figure 2). When the treatment involved own eggs, 20 cycles were deferred and 8 were fresh. In the case of egg donation, there were 97 deferred cycles and 36 fresh cycles (Figure 3).
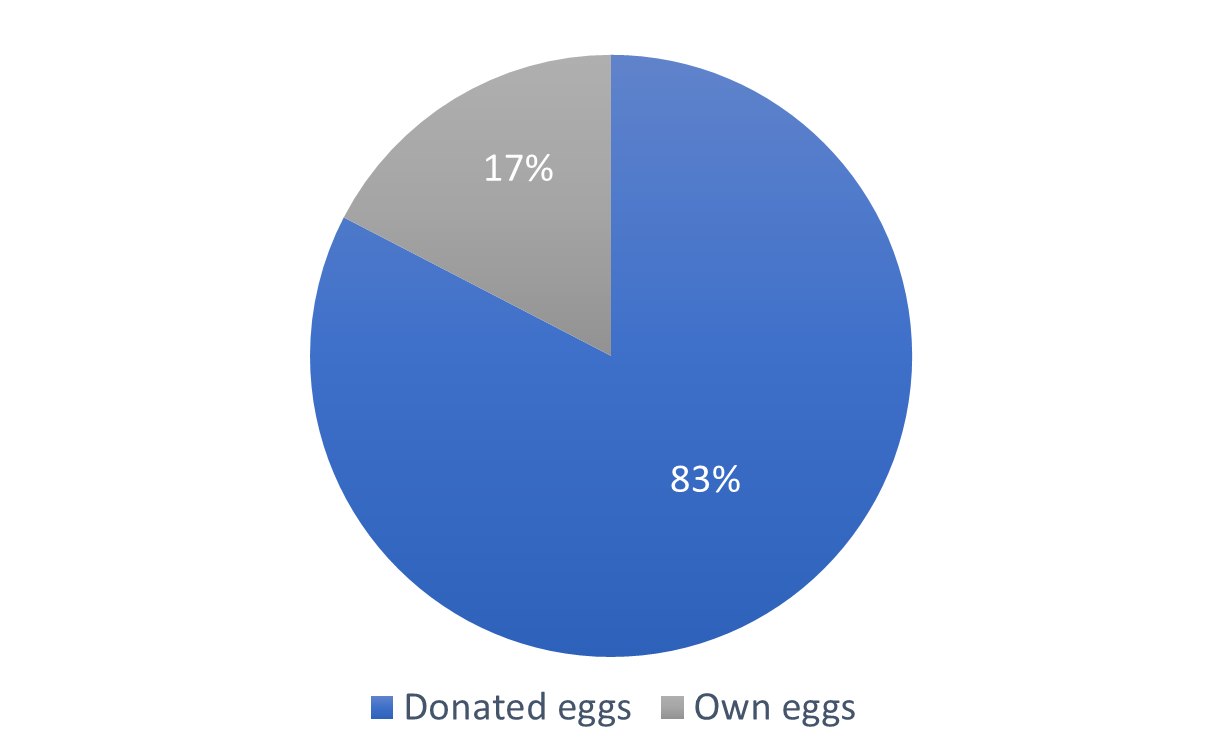
Figure 2. Oocyte origin.
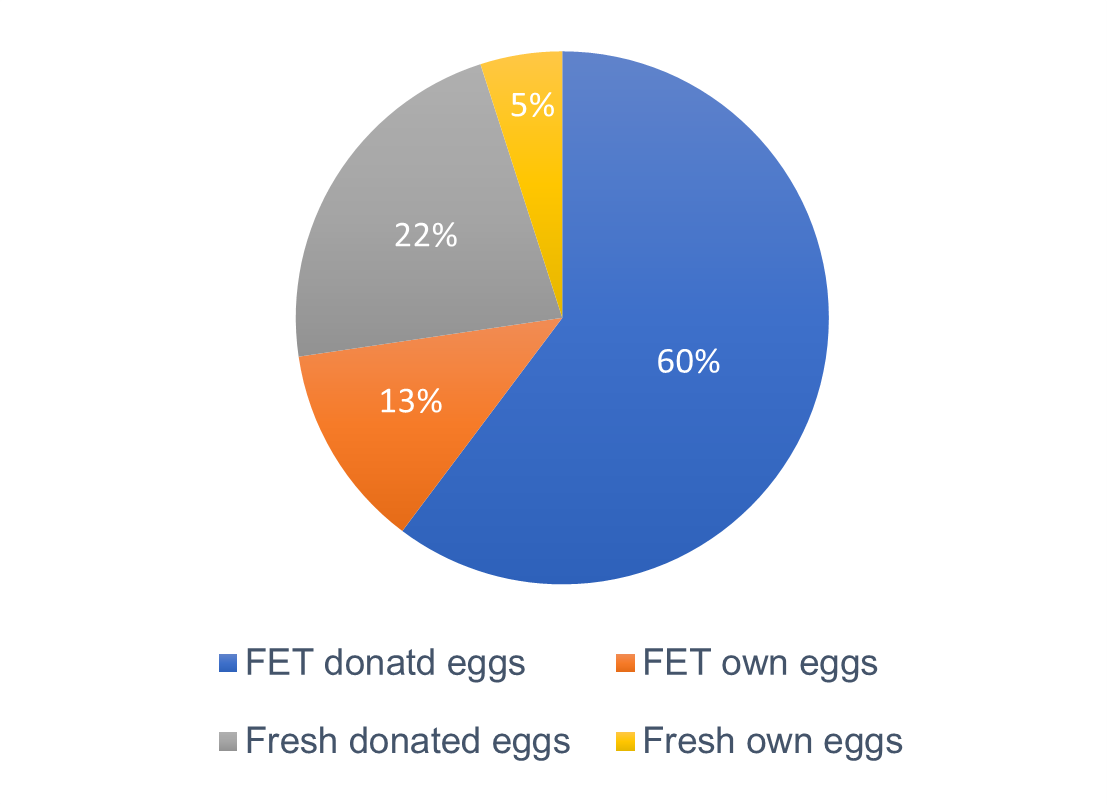
Figure 3. Treatment – Embryo transfer (ET) type.
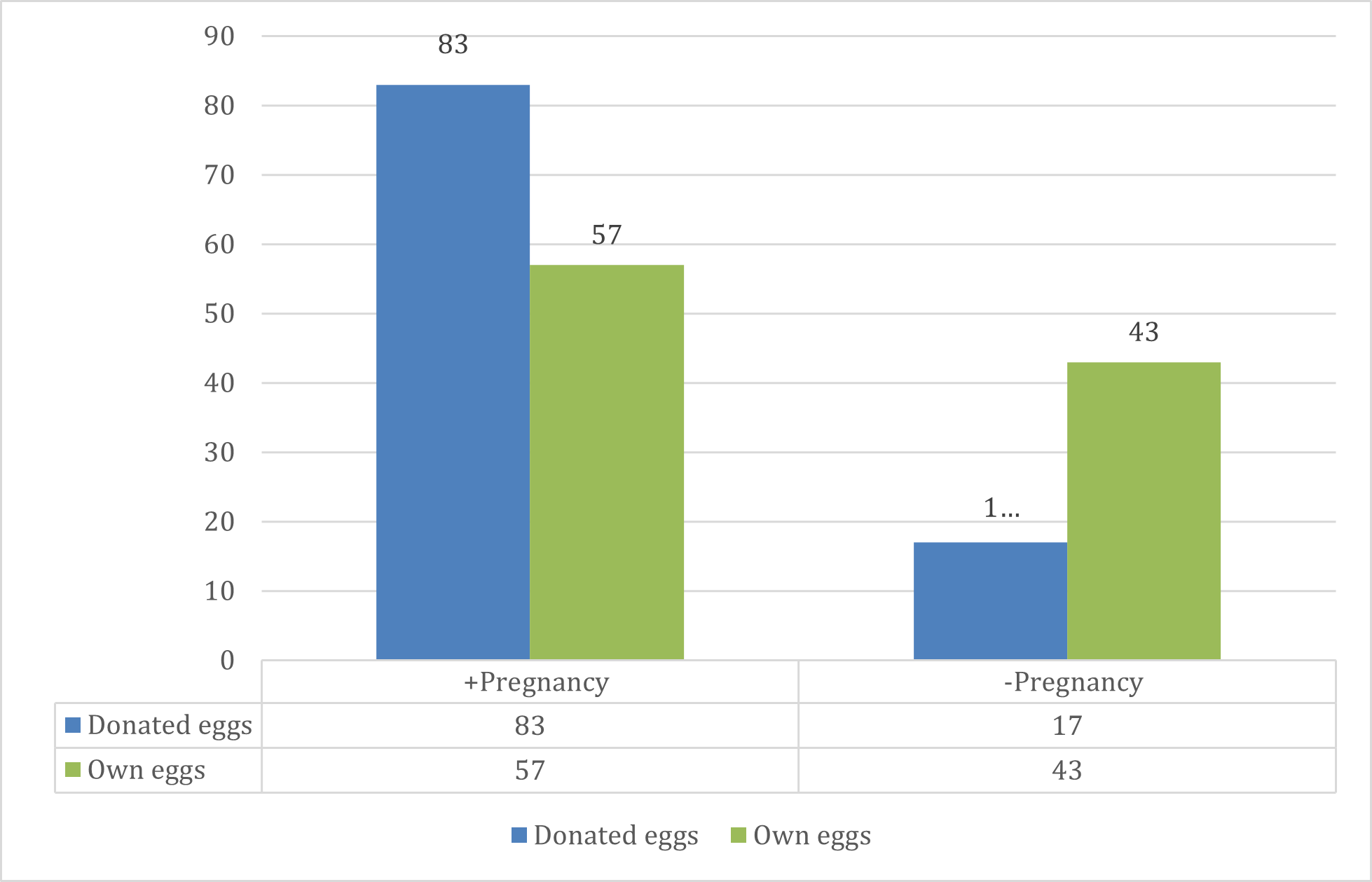
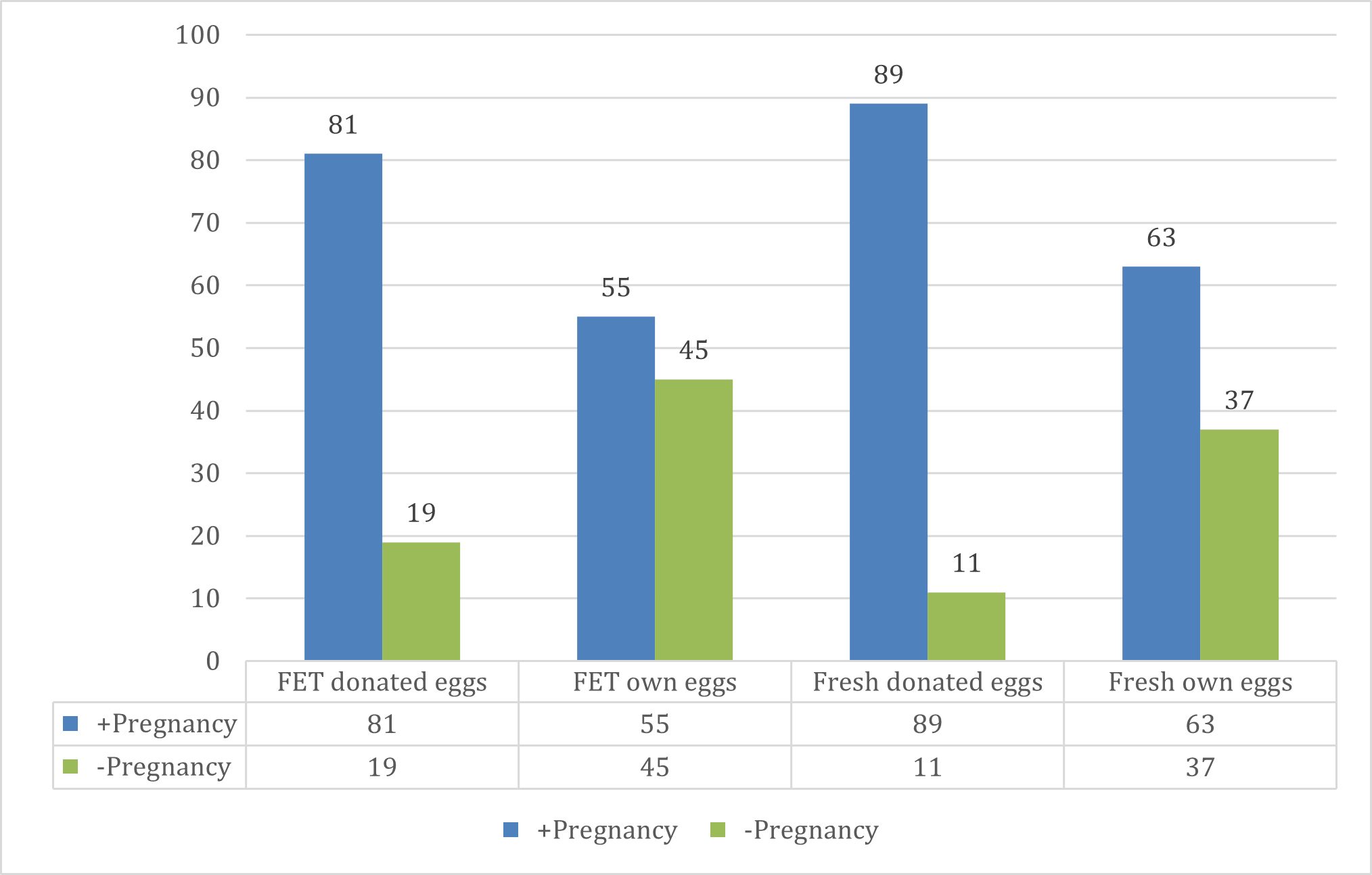
Pregnancy rate with donated oocytes was significantly higher when compared with own eggs (Table 4 & Figure 4). Subgroup analysis revealed that the pregnancy rate with own eggs in fresh cycles was 63%, and when previously cryopreserved embryos were transferred (FET), the pregnancy rate was 55%. When donated oocytes were used in fresh cycles, the pregnancy rate was 89%, and with previously cryopreserved embryos, it was 81% (Table 4 & Figure 5). Pregnancy rates were significantly higher in donated oocytes, irrespective of the type of embryo transfer technique utilized (OR=5.19, p=00009) (Table 4). On logistic regression analysis, the only factor influencing successful pregnancy was the type of eggs used (donates vs own). Other factors including age, type of couple and diagnoses did not show any significant association with successful pregnancy.
|
+Pregnancy (n=127) |
-Pregnancy (n=34) |
OR (95%CI)* |
p-value* |
| Oocyte source |
| OD (n=133) |
111 (83) |
22 (17) |
5.19 (1.98-13.96) |
0.0009 |
| OWN (n=28) |
16 (57) |
12 (43) |
| Type of Treatment/Embrio Transfer (ET) |
| Crio OD (n=97) |
79 (81) |
18 (19) |
4.78 (1.61-14.51) |
0.0051 |
| Crio OWN (n=20) |
11 (55) |
9 (45) |
| Fresh OD (n=36) |
32 (89) |
4 (11) |
7.28 (1.08-49.46) |
0.0412 |
| Fresh OWN (n=8) |
5 (63) |
3 (37) |
Data shown as n(%) *Logistic regression model and Odds Ratio (OR) calculations.
Table 4. Factors associated with successful pregnancy
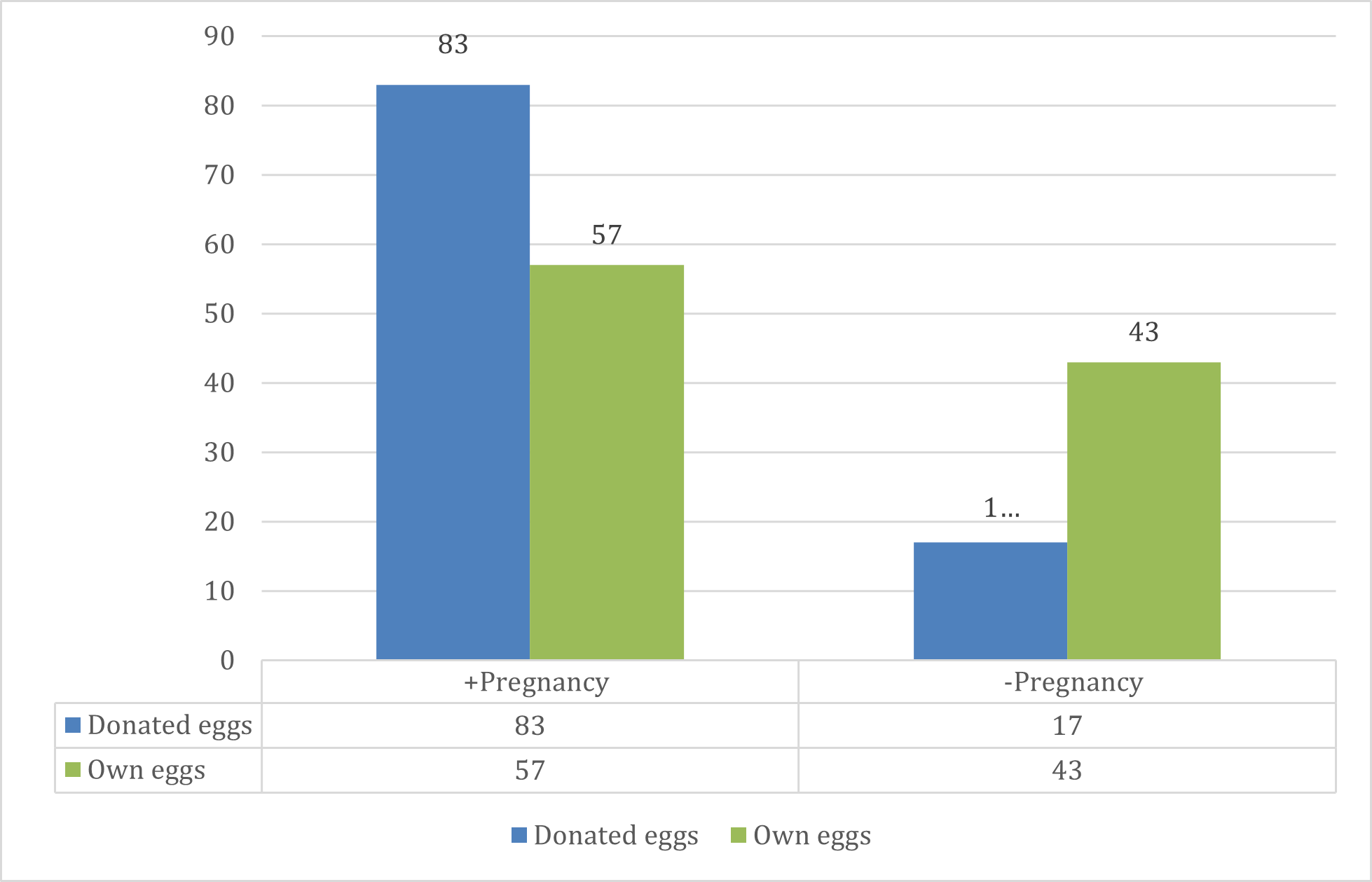
Figure 4. Oocyte source in successful pregnancy vs unsuccessful pregnancy.
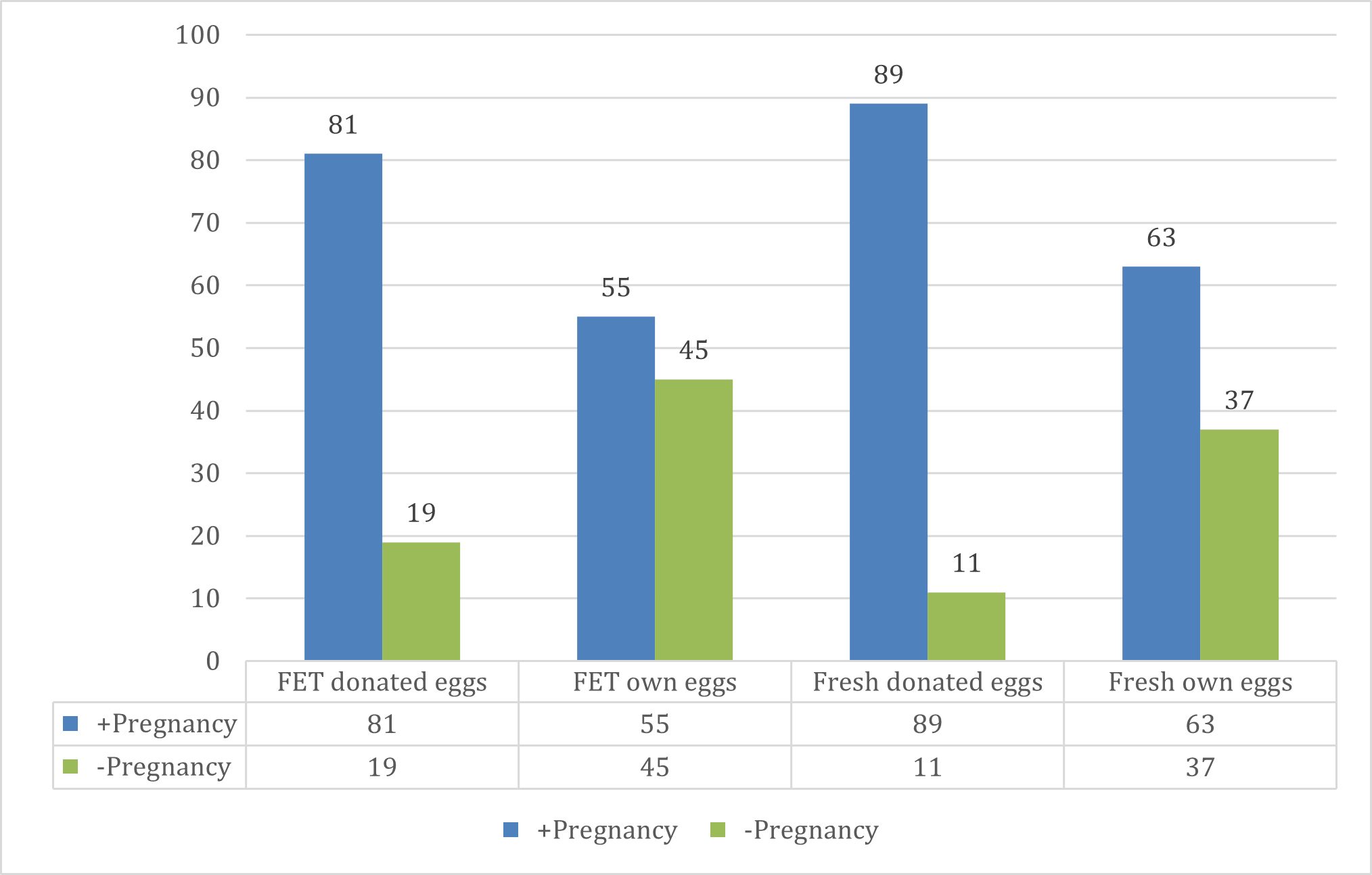
Figure 5. Type of ET in successful pregnancy vs unsuccessful pregnancy.
We reviewed pregnancy outcomes on the 127 pregnancies that were achieved. Twenty-six pregnancies were ongoing (surpassed 20 weeks) at the time of this publication, 33 pregnancies resulted in miscarriage (26%), with 3 ectopic pregnancies, 62 pregnancies resulted in a live birth. So far, there have been 62 confirmed deliveries with a total of 64 children born (5 gestational carriers had elective double transfers). There were 3 fetal deaths (2 due to premature rupture of membranes at weeks 21 and 22, respectively) and 1 at week 36 with no diagnosis (Table 5).
|
N |
% |
| BIOCHEMICAL ABORTION |
8 |
6 |
| MISCARRIAGE |
25 |
20 |
| ECTOPIC PREGNANCY |
3 |
2 |
| ONGOING PREGNANCY |
26 |
20 |
| FETAL DEATHS |
3 |
2 |
| LIVE BIRTH |
62 |
49 |
| Total |
127 |
100 |
Table 5.Pregnancy Outcomes.
No conflicts were reported between the gestational carriers and the intended parents, and all babies are registered in the names of the procreational parents.
Discussion
Argentina has become an attractive option for gestational surrogacy, for both local and foreign patients, due to its openness to new family structures without discrimination based on gender, sex, origin, or ethnicity. In a global context where many countries restrict possibilities for foreign patients, Argentina provides legal and medical security for these treatments.
The multidisciplinary team has proven to be essential in approaching and monitoring these patients. The collaborative efforts of a team established from the outset, all within the same institution in continuous communication, guarantee that Halitus' program delivers personalized treatment to each patient. This approach involves professionals—doctors, nurses, embryologists, psychologists, and lawyers—coming together, sharing insights and experiences to provide the best for our patients.
Although there has been a constant increase in consultations over the years, only a small percentage of patients seeking advice can finally undergo treatment, possibly due to economic, ethical, or social factors. Our retrospective review did not allow for the identification of these factors.
Contrary to popular belief, surrogacy is not exclusive or mostly requested by same-sex couples or single men. In fact, data shows that heterosexual couples, especially those with medical issues related to uterine dysfunctions, are the ones who most often turn to these techniques. However, as shown in our analysis, a higher percentage of male individuals seeking consultation undergo the treatment, compared to heterosexual couples or single women (20 vs 11%).
As described, pregnancy rates with egg donation are higher than those with own eggs. Despite this, pregnancy rates with own eggs were very acceptable in this cohort (57%).
Another consideration to take into account is the risk of multiple pregnancies. In the United States, the transfer of two or more embryos is done in almost 80% of cycles with surrogates, and less than 20% opt for elective single embryo transfer [10]. Although transferring more than one embryo is discouraged due to the risk of multiple pregnancies, there are special considerations that support it. In our intervention model, this and other specificities are addressed both medically and psychologically. In these consultations surrogates and intended parents, with proper guidance, can make decisions regarding the number of embryos to transfer. In our cohort from the 161 treatments, 5 (3.1%) resulted in twin pregnancies that led to 9 live births (one baby died postpartum due to complications from prematurity).
Conclusion
Gestational surrogacy is a global trend that sparks controversies and ethical debates. Despite this, it stands as a beneficial procedure, with a high success rate and a comparatively low risk of complications.
Considering the possibility of human life gestating outside the maternal womb, involving the participation of others, gives rise to arguments both in favor and against. While some question the ethics of exposing gestational carriers to the risks of being pregnant with no procreational desire of their own, other voices defend a woman's right to choose what to do with her own body.
Arguments in favor of LGBTQ+ rights and the capacity of mentally competent adults to collaborate in creating life also align with this perspective.
It is crucial to establish relevant regulations to protect all involved parties, especially unborn children. Beyond the controversy, it is undeniable that gestational surrogacy is a concrete solution that brings hope to those who have lost gestational capacity or harbor the desire for a child.
In the professional field dedicated to this practice for decades, efforts persist to establish the legitimacy of gestational surrogacy within an interdisciplinary team working collaboratively within the same institution. This involves integrating medical, psychological, and legal expertise, prioritizing ethics, respect for human beings, and adherence to the law as regulatory frameworks. The findings from this study, reflecting the experience of our center, indicate that this can be achieved with high rates of success, when performed by a multidisciplinary and experienced team.