Manuscript
Introduction
The endometrium is a complex and dynamic tissue composed of epithelial cells, both luminal and glandular, surrounded by supporting stromal cells, together comprising the innermost layer of the uterus. The primary function of the uterus is supporting fertility, and the endometrium is the layer critically involved in receiving an embryo, facilitating implantation and decidualization, and supporting embryo growth and development until placentation. The adequate development of the endometrium is considered essential for the window of implantation (WOI)[1], and adverse reproductive outcomes, such as implantation failure[2,3] and miscarriage, may be caused by altered proportions during the WOI.
The abnormalities of the endometrium, such as endometriosis[4,5,6,7], hyperplasia[9] and endometrial cancer[9,10,11,12] are traditionally diagnosed using transvaginal ultrasound (TVUS)[13,14] and endometrial histologic[15,16,17,13,2,18]. However, the manual segmentation of the endometrium is subject to subjectivity and prone to errors, especially by inexperienced sonographers.
The study of the endometrium plays a critical role in women's health and reproductive medicine, offering insights into various gynecological conditions and enhancing fertility treatments. Recent advancements in technology, particularly in artificial intelligence (AI)[19,20,14] have revolutionized how endometrial studies are conducted and interpreted.
The important role of ultrasound in female reproductive function is evaluation of ovarian reserve (OR)[21,4] and endometrial receptivity (ER)[19,22,21,2]. In the assessment of OR, serial ultrasound examinations can provide reliable markers to follicular monitoring[21], the diagnosis of Polycystic Ovary Syndrome (PCOS)[21,2,3], and prediction of oocyte quality and pregnancy outcomes, such as ovarian follicular diameter and volume, number of follicles, ovarian stromal blood flow index, etc.
For ER, endometrial thickness[19,22,3] and volume, endometrial morphology[21], and spiral arterial blood flow index[21] are effective evaluation indicators.
Materials and Methods
This section provides an overview of the methodologies and materials employed in this comprehensive analysis on various aspects of endometrial health and disease, with a focus on advanced AI and machine learning techniques. Detailed methodologies are described for five key areas of analysis: Endometrial Hyperplasia and Endometrial Cancer, Endometriosis, Endometrial Receptivity, AI for Identifying Endometrial CD138+ Cells in PCOS and Recurrent Implantation Failure, and the overall Role of AI in Endometrial Studies. In each subsection, the application of convolutional neural networks (CNNs) and other AI models is detailed, along with data sources, patient cohorts, and validation techniques. Diagnostic accuracy is enhanced, treatment outcomes are improved, and the complex molecular and structural features of the endometrium are understood through these methodologies. Various data types, including histopathological images, MRI scans, and transcriptomic profiles, are integrated to offer comprehensive insights into endometrial conditions, support non-invasive diagnostics, and facilitate personalized treatment strategies. Technological advancements and techniques, diverse datasets and features, and rigorous classification and validation criteria are highlighted to ensure the reliability and robustness of the findings.
Endometrial Hyperplasia and Endometrial Cancer
Recent advancements in AI and ML have revolutionized the diagnosis of endometrial hyperplasia and endometrial intraepithelial neoplasia. Convolutional neural networks (CNNs) developed from histopathological images are used to screen and diagnose these conditions, improving diagnostic accuracy and reducing subjective interpretation variability. The interpretable deep learning pipeline, im4MEC[23], predicts molecular classifications of endometrial cancer from whole-slide images, further enhancing diagnostic capabilities.
Artificial intelligence (AI) in medicine encompasses the application of knowledge- and data-intensive computer-based solutions for disease prevention, diagnosis, and treatment. One of its pivotal domains is medical imaging, which has seen continuous evolution since its inception in the mid-twentieth century.
Efforts to improve diagnostic accuracy and automation in medical image analysis, particularly for the diagnosis and classification of endometrial cancer using convolutional neural networks (CNNs) and other advanced models, have been concentrated on.
Role of CNNs in Medical Image Analysis:
CNNs extract complex features from medical images, particularly whole-slide images (WSIs) in endometrial cancer diagnosis. Morphological features correlating with molecular subtypes are identified by CNNs, reducing pathologist workload. Advanced models like G2LNet[8] and im4MEC[23] facilitate precise lesion identification through feature extraction, fusion, and predictive analysis. Integration of radiomics and deep learning enables non-invasive prediction of tumor characteristics, showcasing AI's potential in gynecological healthcare.
Technological Advances and Techniques:
Models such as DeepLab v3[10], ResNet-50[10], HIENet[17], YOLOv3[11], and MoCo-v2[24] are employed for tasks such as lesion detection, self-supervised learning, and enhancing diagnostic performance. Spectroscopic techniques and DNA methylation analysis[25] combined with machine learning identify biomarkers critical for diagnostics.
Data Sources and Features:
Datasets include diverse medical imaging (histopathological images[17,26,13], WSIs[27,10,23], MRI scans[9,28,29,30] and clinical data. Key features for training CNN models include textural patterns, shape, intensity variations, and morphometric characteristics. Cellular structures, tissue architecture, glandular morphology, nuclear atypia, and radiomic features are commonly analyzed.
Patient Cohorts and Clinical Context:
Patients encompass various stages and subtypes of endometrial conditions, providing comprehensive training and validation contexts. Clinical features such as age, CA125 levels[18], tumor size, grade, menopausal status[30], BMI[29,25,31], and family history are considered. Specific diagnostic procedures and annotations by expert pathologists enrich the clinical relevance of the imaging data.
Classification and Validation:
Endometrial hyperplasia and neoplasia are classified based on image features, while molecular subtypes guide endometrial cancer classification. Risk groups are determined using ESGO/ESMO/ESP guidelines, integrating whole-lesion segmentation on MRI images and statistical methods like random forest[28,31] and LASSO[9,29,18]. Survival predictions (5-year PFS)[29] utilize radiomics features from MRI scans combined with clinical and MRI risk factors. Validation metrics include accuracy, sensitivity, specificity, AUC-ROC, precision rate, positive and negative predictive values, and clinical outcome comparisons. Techniques like cross-validation[28,23,17,26,13,31], ROC analysis[12], Kaplan-Meier analysis[9], Cox models[9], and biomarker validation[2,18,32,31] ensure robust model validation and reliability.
Endometriosis
Studies related to endometriosis were analyzed to determine correlations, classification criteria, models applied, data quality, quantity and specific features, cohorts, validation criteria, and clinician validation.
Diverse AI and Machine Learning Approaches in Medical Diagnostics for Endometriosis:
The ability of Convolutional Neural Networks (CNNs) to analyze medical images and support non-invasive diagnostics for endometriosis is the focus of many studies. A variety of models and techniques are explored in other research, including Artificial Neural Networks (ANNs) for proteomic data analysis[33], logistic regression[6,20,14], decision trees[34], Random Forest[6,20,34,14], eXtreme Gradient Boosting[6, 20], and Support Vector Machines (SVMs)[14] for classification and predictive modeling. Genetic algorithms[7] and mass spectrometry[5,7] are also utilized for diagnostics, with peptide profiling[5] and protein expression[7] analysis being leveraged. The broader landscape of AI and machine learning in medical diagnostics is highlighted by these diverse methodologies, where imaging tasks are excelled in by CNNs, and significant benefits for data analysis and pattern recognition in molecular and cellular biology are offered by other models.
Technological Advances and Techniques:
A range of AI and machine learning techniques for endometriosis diagnostics have been employed, including CNNs for imaging, ANNs for proteomic data analysis, logistic regression, decision trees, Random Forest, eXtreme Gradient Boosting, SVMs for classification and predictive modeling, and genetic algorithms and mass spectrometry for diagnostics, with peptide profiling and protein expression analysis highlighted.
Data Sources and Features:
A range of datasets, including urine, plasma, serum samples, MRI, and histopathological images, is utilized in various studies. Peptide profiles[5] are analyzed from urine samples, while proteomic[5,7] and metabolomic[35] data are processed from serum samples. MRI datasets[6,35], annotated for endometriosis, emphasize tissue characteristics and lesion specifics. Numerical, categorical, and text data focusing on symptoms, diagnosis, and treatment are collected from clinical records. RNA-seq and methylomics data[34,36] are included in some datasets, while digital histopathological images[37] are used in others, with textural, structural, and morphometric features extracted by CNN models. The diversity of data features highlights the need for standardized data collection and analysis protocols, encompassing hormone profiles[4], miRNA[6], metabolite levels[38,35], and genetic variables[14].
Patient Cohorts and Clinical Context:
Individuals with dysmenorrhea, pelvic pain, and infertility, including those diagnosed with endometriosis, were included in the patient cohorts. Clinical data such as age, symptoms, and surgical history were incorporated into MRI datasets. Plasma samples were collected from women with chronic pelvic pain, confirmed by laparoscopy or MRI. Hormonal profiles and ovarian reserve markers characterized subfertile women. Increased metabolite levels in endometriosis patients were indicated by serum samples. Endometriosis stages, age ranges, and symptoms like dysmenorrhea and infertility were included in proteomic studies. Comprehensive demographic, symptom, and treatment data were provided by the Ziwig Health[20] platform.
Classification and Validation:
Various methods have been used to classify endometriosis in studies, including peptide diagnosis, CNN-classified images, sensitivity, specificity, AUC, hormone levels, and spectra analysis. Protein expression[7], spectral shifts[35], serum protein patterns[7], clinical features[14], age, colorectal involvement, likelihood of live birth, microbiota composition[3], and genetic data[14] have also been utilized. Models were validated using metrics such as sensitivity, specificity, F1-score, and AUC. Cross-validation methods included random datasets, 10-fold splits, and 70/30 training-validation divisions. Statistical methods like t-tests, ROC analysis, and biomarker assessment were employed. Specific validation results included 90.9% sensitivity and 92.9% specificity from urine samples, and 86% classification accuracy with 100% specificity and 58.3% sensitivity using an 80/20 cross-validation.
Endometrial Receptivity:
AI models predict success rates of fertility treatments and assess endometrial receptivity, addressing challenges in assisted reproductive technology. Integration of proteomics, metabolomics, and transcriptomics with AI provides novel insights into disease mechanisms and improves clinical outcomes in gynecological healthcare.
Studies related to endometrial receptivity were analyzed to determine correlations, classification criteria, applied models, data quality, quantity, specific features, cohorts, validation criteria, and clinician validation.
The application of convolutional neural networks (CNNs) and other AI models in endometrial studies is varied based on the study's focus and data type. While CNNs are not specifically mentioned in some studies, various AI models, including machine learning algorithms, are often used to analyze transcriptomic[39,16] and gene expression data[39,1]. A crucial role in studies involving image analysis, such as histological image[15] segmentation and classification, where models like Attention U-Net and GoogLeNet Inception[19] are used to significantly enhance accuracy. In studies where transcriptomic analysis of gene expression profiling is the primary focus, traditional AI and machine learning techniques are more commonly used to interpret complex data and identify patterns related to endometrial receptivity and fertility treatment outcomes.
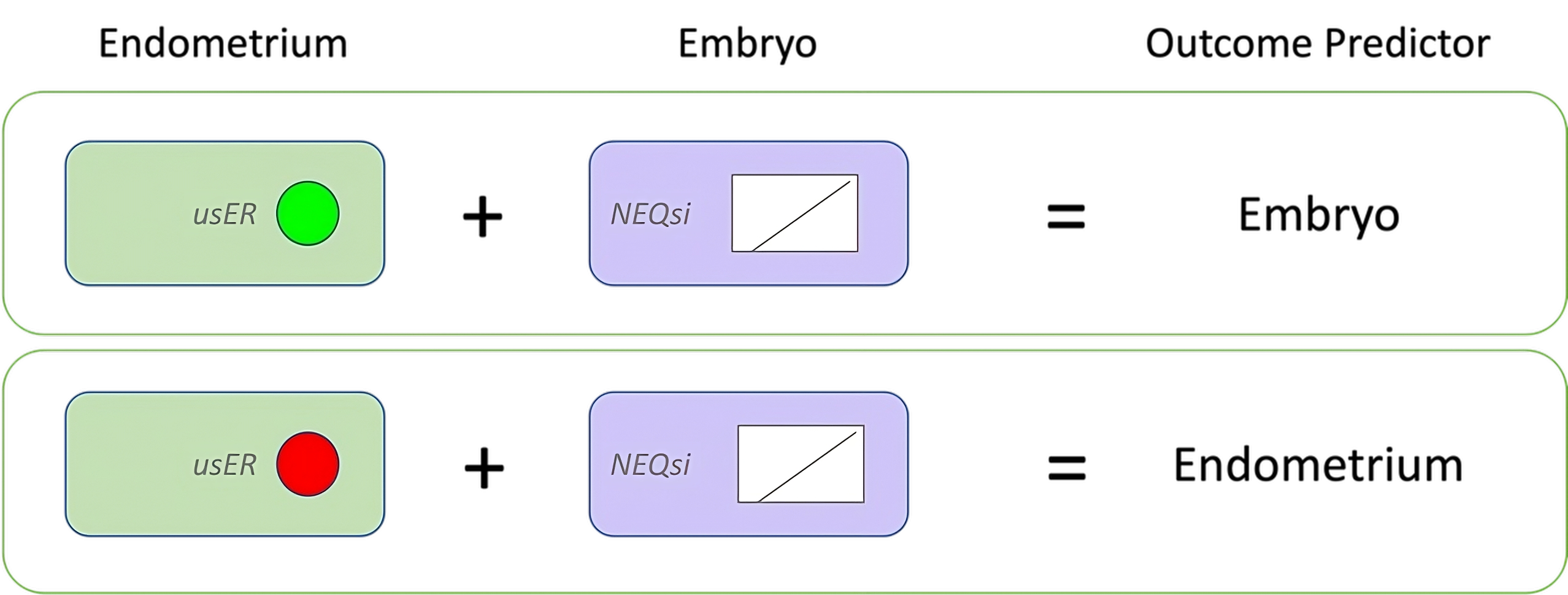
Endometrial images were classified as "good" or "bad" based on features such as external layer thickness and echogenicity, following the Asch endometrial grading system[22]. The endometrium was classified into six categories by this novel system, which were then used to train our AI model, Endoclassify. The endometrial structural features were assessed, images were classified, and endometrial receptivity was predicted by this AI model without clinical intervention, achieving a high degree of correlation with clinical outcomes.[Figure 1].
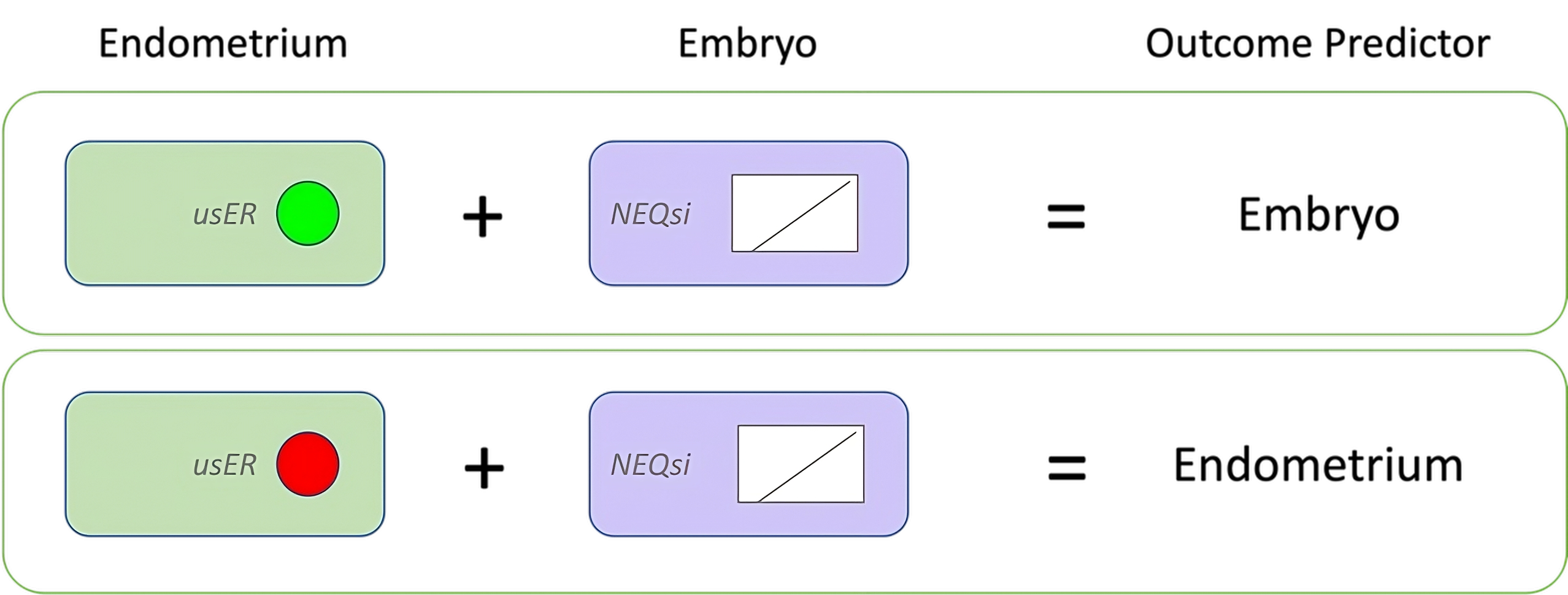
Figure 1. Asch Endometrial Grading System.
In our previous study[19], clinical outcomes of two categories—fresh and frozen embryo transfer cycles—were analyzed, demonstrating significant pregnancy success rates within these groups. Building on this foundation, the current analysis has been expanded to introduce two new categories related to assisted reproductive technology (ART): OD (Oocyte Donation cycles) and GS (Gestational Surrogacy cycles) [Table 1]. The inclusion of these categories is intended to enrich the understanding of pregnancy outcomes and further validate the efficacy of different ART methods.
|
| 1 A α |
1 B α |
1 A β |
1 B β
| Patients (n) |
| FRESH |
80 |
40 |
14 |
7 |
141 |
| FROZEN |
93 |
27 |
6 |
4 |
130 |
| OD |
100 |
30 |
14 |
9 |
153 |
| GS |
80 |
10 |
4 |
2 |
96 |
| TOTAL |
353 |
107 |
38 |
22 |
520 |
Number of cases according to endometrial classification
(Fresh cycles / Frozen cycles / OD Oocyte Donation cycles / GS: Gestational Surrogacy cycles).
Table 1
Oocyte donation (OD) and gestational surrogacy (GS) are increasingly utilized in reproductive medicine, providing viable options for individuals and couples facing infertility.
In this expanded study, clinical data from 520 patients were analyzed, categorized into four groups: fresh cycles (141 patients), frozen cycles (130 patients), OD cycles (153 patients), and GS cycles (96 patients). The number of cases according to endometrial classification and the corresponding pregnancy rates were assessed. The goal was to demonstrate that the extended categories (OD and GS) not only reach but also excel in pregnancy outcomes, similar to the previous findings with fresh and frozen eggs.
The new data presented in this study underscore the importance of expanding the analysis to include OD and GS cycles. By doing so, a more comprehensive understanding of ART success rates is sought, providing valuable insights into the effectiveness of these reproductive technologies [Table 2].
|
| 1 A α |
1 B α |
1 A β |
1 B β
| Pregnancies (%) |
| FRESH |
59 |
74% |
20 |
50% |
1 |
7% |
0 |
0% |
80 |
57% |
| FROZEN |
70 |
75% |
13 |
48% |
1 |
17% |
0 |
0% |
84 |
65% |
| OD |
75 |
75% |
20 |
67% |
7 |
50% |
0 |
0% |
102 |
67% |
| GS |
62 |
78% |
7 |
70% |
2 |
50% |
0 |
0% |
71 |
74% |
| TOTAL |
266 |
|
60 |
|
11 |
|
0 |
|
337 |
|
The pregnancy rates in patients of the four groups (Fresh-Frozen-Oocyte Donation and Gestational Surrogacy cycles)
that belong to Asch classification 1Aα and 1Bα are significantly higher than of all other groups in the study (p <= than 0.05).
Table 2
It is suggested that the inclusion of OD and GS categories enhances pregnancy outcomes, further supporting their integration into clinical practice. Our Endoclassify AI model[19] has been instrumental in accurately identifying and classifying these new categories, ensuring that the right outcomes are achieved. This advanced AI technology has demonstrated its capability to effectively analyze and predict successful pregnancies across diverse ART methods, thereby reinforcing the reliability and applicability of these innovative reproductive techniques.
The normalization of data management across the studies reveals that the datasets are primarily composed of either transcriptomic data or high-resolution images of endometrial samples, with some studies utilizing augmented ultrasound images. Gene expression profiles for transcriptomic datasets and segmentation or histological markers for imaging datasets are generally included as data features. An understanding of molecular environments is emphasized by the studies focusing on transcriptomic data, while structural and classification features of the endometrium are concentrated on by imaging studies. Where applicable, image features include the segmentation of endometrial layers, glandular structures, and stromal density.
Regarding patient features, women of reproductive age undergoing fertility treatments are involved in most studies, with specific inclusion criteria such as age ranges (typically up to 40 years old) and clinical backgrounds (e.g., history of infertility, recurrent implantation failure, or specific outcomes of previous ART cycles). Demographic details, clinical histories, and treatment outcomes are commonly included to correlate with the molecular or structural data being analyzed. Homogeneity in patient populations is generally ensured through detailed inclusion and exclusion criteria, often focusing on patients without known endometrial pathologies or systemic diseases.
The classification criteria are based on differentiating between receptive and non-receptive endometrium using transcriptomic profiles[39] to determine the optimal timing for embryo transfer; endometrial images are classified as 'good' or 'bad' based on segmentation and classification models[19]; histological features[15] relevant to endometrial receptivity and fertility outcomes are classified by the CNN model; specific gene expression profiles are identified to distinguish between receptive and non-receptive endometrium states for personalized embryo transfer protocols; gene expression profiles are compared between natural and stimulated cycles during the window of implantation.
The validation criteria include metrics such as accuracy, sensitivity, specificity, and other relevant metrics to ensure the reliability of the AI-based transcriptomic testing; accuracy (95%), loss (10%), sensitivity (93%), and specificity (93%) are included; model performance is validated using a hold-out dataset to ensure reliability and robustness; gene expression profiles are compared between patients with successful and unsuccessful implantation outcomes using statistical methods to validate the predictive power of identified biomarkers; differential expression of selected genes is confirmed using quantitative real-time PCR (qRT-PCR).
AI for Identifying Endometrial CD138+ Cells in PCOS and Recurrent Implantation Failure:
The anovulatory PCOS samples exhibited significantly lower CD138+ cell percentages than PE PCOS samples, with phenotype A PCOS showing higher percentages than phenotype D. Interestingly, CD138+ cell percentages were unaffected by endometrial receptivity status in RIF samples[2,3].
The estradiol-mediated recruitment of CD138+ cells from systemic circulation into the PE is suggested, potentially explaining the higher concentrations observed. However, further investigation into estrogen receptor expression and sensitivity dynamics across the menstrual cycle is warranted, due to lower CD138+ cell percentages in anovulatory PCOS despite comparable endometrial thickness.
Despite limitations such as a lack of confirmed chronic endometritis cases and incomplete clinical data for RIF patients, the AI-algorithm training and validation for identification of endometrial CD138+ cells in infertility-associated conditions, including polycystic ovary syndrome (PCOS) and recurrent implantation failure (RIF), demonstrates the AI's efficacy in rapid, reproducible assessment of endometrial CD138+ plasma cells. Larger datasets and prospective study designs should be explored in future research to validate AI's role in assessing endometrial inflammation and optimizing reproductive health outcomes.
Role of AI in Endometrial Study:
Artificial intelligence (AI) technology has made significant strides in the medical field, yet its application in assessing female reproductive function remains at an early stage. Ethical concerns surrounding AI, including issues of responsibility and transparency in AI processes and human-machine interaction, pose challenges such as ethical, liability, and legal risks. These issues can contribute to patient and clinician distrust of AI, especially concerning data privacy and security, with many patients hesitant to consent to data uploading for intelligent analysis.
Moreover, the effectiveness of AI models is heavily influenced by data quantity, quality, and diversity. Small sample sizes, inadequate sample diversity, or imbalanced data ratios can introduce bias into models, limiting their generalization and practical applicability, particularly in the complex realm of female reproductive evaluation. Ensuring high-quality images and accurate data collection methods are crucial prerequisites for achieving accurate AI evaluations. Multicenter studies are essential to expand sample sizes and enhance model robustness and generalizability across different institutions and machine types.
Standardization of evaluation criteria and data storage methods among institutions is paramount to address variability in assessing female reproductive function. While AI has demonstrated potential to match or surpass expert performance in some areas, its role should be viewed as complementing rather than replacing clinicians. AI's strength lies in screening and early warning systems, augmenting clinical decision-making rather than supplanting it. Clinicians must critically evaluate AI model construction and ensure alignment with real-world clinical scenarios to optimize patient care.
Results
In the domain of artificial intelligence models, advancements in endometrial studies are facilitated through the proposal of multi-level frameworks tailored to specific areas of research. This paper explores the integration of diverse technologies to enhance the analysis of endometrial receptivity during Assisted Reproductive Technology (ART) procedures. By combining transcriptomic data, segmented ultrasound images, high-resolution histopathological images, and comprehensive patient clinical data, a multi-omics approach is advocated. This integration enables correlation of clinical outcomes with molecular and structural features, thereby improving the understanding of endometrial receptivity and facilitating biomarker discovery for enhanced predictive capabilities in ART outcomes.
Furthermore, this study introduces Endoclassify[19], a novel method utilizing transvaginal ultrasound images to objectively evaluate endometrial conditions. Employing rigorous criteria, Endoclassify categorizes images into ‘Good’ or ‘Bad’ and quantifies the likelihood of pregnancy for each classification. These insights equip clinicians with essential information for informed decision-making regarding embryo transfer or cycle postponement.
Moreover, for enhancing endometrial cancer analysis, the integration of convolutional neural networks (CNNs) such as G2LNet, im4MEC, and HIENet with radiomics-based nomograms and traditional machine learning algorithms is proposed. Advanced detection techniques and self-supervised learning models complement these approaches, aiming to improve feature extraction, biomarker identification, and predictive modeling accuracy.
In the context of endometriosis, a multi-modal AI approach is recommended, leveraging CNNs for imaging data analysis, machine learning algorithms for clinical and molecular data integration, and ensemble methods for robust predictive outcomes. Logistic regression and partial least squares discriminant analysis play roles in initial variable selection and relationship understanding, contributing to comprehensive insights into this complex condition.
These integrated solutions illustrate the potential of artificial intelligence to advance understanding and management across diverse facets of endometrial studies, from reproductive health and cancer analysis to complex conditions like endometriosis.
Discussion
The best analysis, decision-making, and preparation of the data are required for artificial intelligence models to develop solutions. For these reasons, datasets, data features, image features, and patient cohorts need to be defined. Additionally, classification and validation criteria must be established. Finally, validation by clinical researchers is essential.
For endometrial receptivity, integration of transcriptomic data from ART procedures, alongside high-resolution ultrasound and histopathological images, aims to correlate gene expression and imaging features with clinical outcomes.
In endometrial cancer, a multi-modal approach utilizing histopathological images, MRI scans, radiomics, and proteomic/metabolomic profiles enhances diagnostic accuracy and personalized treatment strategies.
For endometriosis, AI models integrate clinical, imaging, molecular, and histopathological data to predict stages and outcomes, utilizing biomarkers and advanced imaging techniques. Validation across these domains involves rigorous statistical analysis and diverse validation cohorts to ensure robustness and clinical applicability.
Conclusions
This review synthesizes findings on the application of artificial intelligence (AI), particularly convolutional neural networks (CNNs), in enhancing diagnostic and prognostic capabilities across various aspects of gynecological health.
The classification of endometrial patterns (trilinear, semi-trilinear, unilinear) and the analysis of uterine peristalsis are enhanced by AI technologies, surpassing manual methods in accuracy. Quantitative assessment of endometrial vascularization and blood supply is improved using AI, leading to better predictions for pregnancy outcomes. Traditional challenges, such as time-consuming manual measurements and significant inter-observer variability, are mitigated by AI-assisted ultrasound, which provides automated detection and measurement of follicles. Accuracy is further enhanced, examination time reduced, and reproducibility improved in follicular monitoring through segmentation algorithms (e.g., optimal thresholding, edge-based methods, active contour methods) and three-dimensional (3D) ultrasound techniques.
Variability is reduced and diagnostic accuracy in follicular monitoring and endometrial receptivity (ER) assessment is improved by AI models in ultrasound imaging. However, challenges remain, including the need for robust AI models that generalize well across different imaging conditions and equipment. Technical issues must be addressed and model validation across diverse patient populations ensured for AI to be integrated into clinical practice. Future research focuses on enhancing AI algorithms for real-time follicular monitoring and improving ER assessment, with clinical adoption dependent on overcoming current limitations and demonstrating practical benefits in improving ART outcomes.
For endometrial receptivity in assisted reproductive technology (ART), integration of AI with transcriptomic testing and biomarkers shows promise in improving embryo transfer timing and personalized treatment strategies, particularly in patients with recurrent implantation failure. However, challenges such as retrospective study designs and the impact of controlled ovarian stimulation on gene expression profiles are acknowledged.
In endometrial cancer and hyperplasia, AI models, including CNNs and radiomics-powered machine learning, significantly enhance diagnostic accuracy, sensitivity, and specificity. These models improve preoperative risk classification, prognostication, and facilitate personalized treatment planning. Challenges such as data standardization and model interpretability need addressing to maximize clinical utility.
For endometriosis, non-invasive diagnostic methods like proteomic profiling and AI models demonstrate high sensitivity and specificity, potentially reducing the need for invasive procedures. CNNs and machine learning algorithms enhance diagnostic accuracy but require further research to improve specificity and reproducibility.
Collectively, AI models, particularly those leveraging deep learning, show promise in enhancing diagnostic efficiency, predicting molecular subtypes, and improving clinical outcomes across gynecological cancers and reproductive health. Future research should focus on validating these models and integrating them into clinical workflows to optimize patient care.